Step 3: Billing for Fully-Paid Patient Claims
Before you begin
A Fully-Paid Patient Claim is one in which the patient is invoiced the full amount, and pays in full. Then the Practice provides the service of submitting the claim to Medicare on the patient's behalf.
Procedure
- Within the patient's record, select the Accounts margin menu, and then locate and double-click the account you want to bill to.
-
Click

to begin issuing a new invoice. The prompt appears.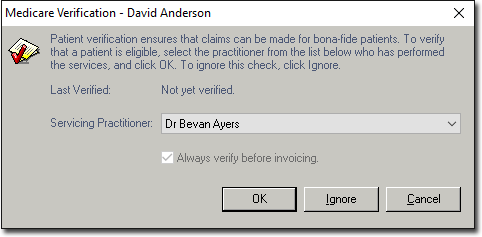
- Click OK if required to verify.
- Click Ignore if already verified.
-
Select the Service Type if required. There will only be multiple service types if you have pre-configured in setup.
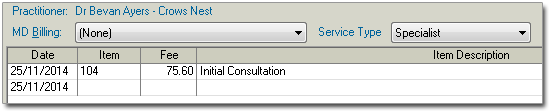
- Enter the appropriate Service Date and ItemNumber as desired. A Service Item's fee will appear automatically. Ensure the fee is correct.
-
Tab to the Service Text field, and then double-click the
field to reveal the
 Ellipsis button. Click this to add text for Medicare if
required, and then click OK. Repeat steps 4-5 if additional
Service Items are required on the invoice.
Ellipsis button. Click this to add text for Medicare if
required, and then click OK. Repeat steps 4-5 if additional
Service Items are required on the invoice.
- Because the patient is paying this account, click Add Receipt.
- When prompted, select the associated Referral, and click Select.
- You will be prompted to enter the date-of-issue for the invoice. The default is the current date.
- Click OK.
-
In the New Receipt window, select the Payment
Method Type (Cash, Cheque, Direct Debit, EFTPOS Manual or EFTPOS Auto
(TYRO), Bank/Card Type, and enter the full payment Amount from
the Patient.
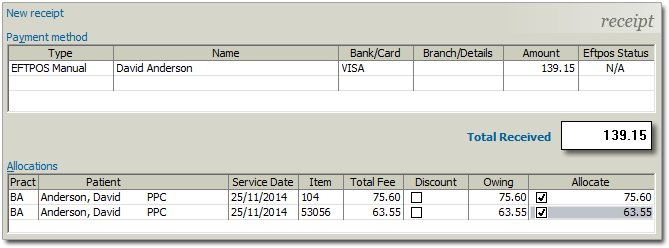
- Allocate the payment amount to the invoice by ticking the check box against each amount owed in the Allocate column.
-
Click Issue. You will be prompted to enter the date-of-issue
for the receipt. The default is the current date.
Important:If your Practice does not use a TYRO Terminal, bypass the next Step
-
Click OK. If the Practice has a TYRO terminal, and has selected a receipt Payment Method of 'EFTPOS Auto', the TYRO terminal (Patient Easyclaim) window will appear. Have the patient swipe their card, select the appropriate account, type and enter their PIN. The online payment process commences and TYRO will print a receipt for the patient.

-
The Print Report window will appear. Ask the patient "Would
you like me to submit the claim to Medicare on your behalf?".
- If Yes, the patient does not require copy. Click the File button to cancel printing.
- If No, the patient decides to claim with Medicare directly. Click the Print button to print an invoice/receipt.
- On the Invoice tab, click the Patient Claim button (located bottom-right).
-
In the New Patient Claim window, select the required
Refund Method of payment. The Refund Method selection
options are as follows:
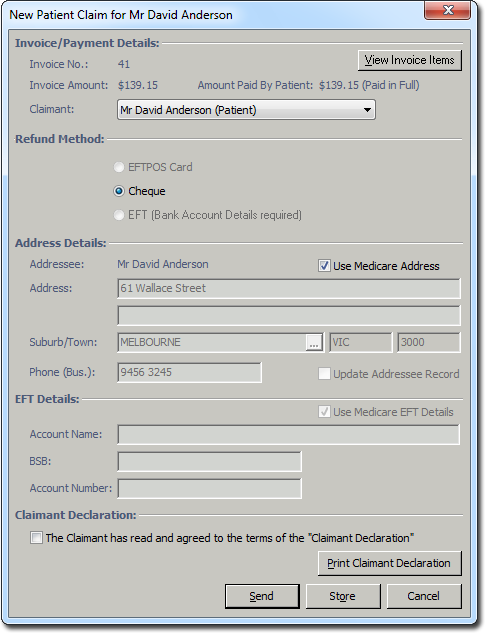
- EFTPOS Card - if the patient's payment is via a card connected to a Savings or Cheque account using a TYRO Terminal, the refund will be reimbursed to the account within ~10 seconds.
- Cheque - if the patient's payment is via a card connected to a Credit Account (Visa, MasterCard) using a TYRO Terminal, or any card via a Merchant Bank Terminal, Cash or Cheque, the claim will be submitted to Medicare. If the patient has bank details logged with Medicare, the cheque will be overridden, and reimbursement will be made to the provided account. If the Patient has not logged bank details with Medicare, Medicare will reimburse via cheque sent to the Patient.
- EFT (Bank Account Details required) - try not to use this Refund Method.
- Set Claimant Declaration and click Send.
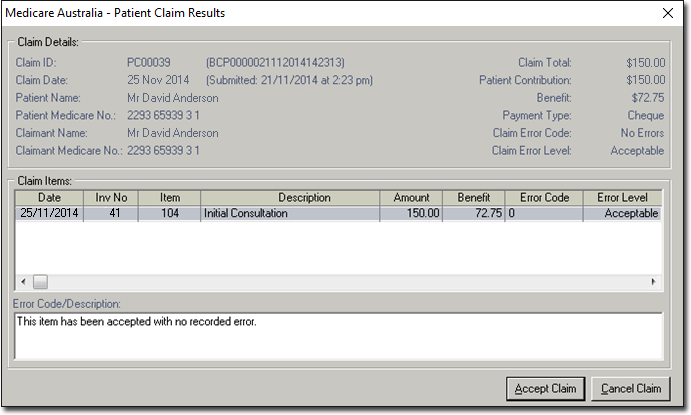
-
In the Patient Claim Results window, click Accept
Claim. This will transmit the claim to Medicare, where the Patient's
banking details are checked.
-
If EFTPOS Card was selected, and the Patient's payment was
from a Savings or Cheque Account through the TYRO Terminal, the TYRO terminal
(Patient Easyclaim) window will re-appear. Have the Patient re-swipe their card,
selecting the appropriate account type, and entering their PIN. The online reimburse
payment process commences. The Patient will be prompted to accept the claim on the
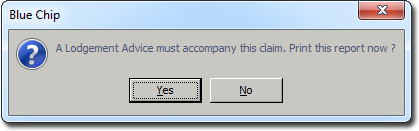
terminal, and then TYRO will print a receipt for the patient. A Lodgment
Advice prompt will appear to print report if required.
Results
On the Invoice tab, notice that the invoice now has a Claim ID, confirming submission. The claim has also been flagged in the Medicare Australia module as a Finalised Receipt Claim (hidden as a processed claim).