Batch Bulk Bill Claim (without TYRO) to Medicare
Before you begin
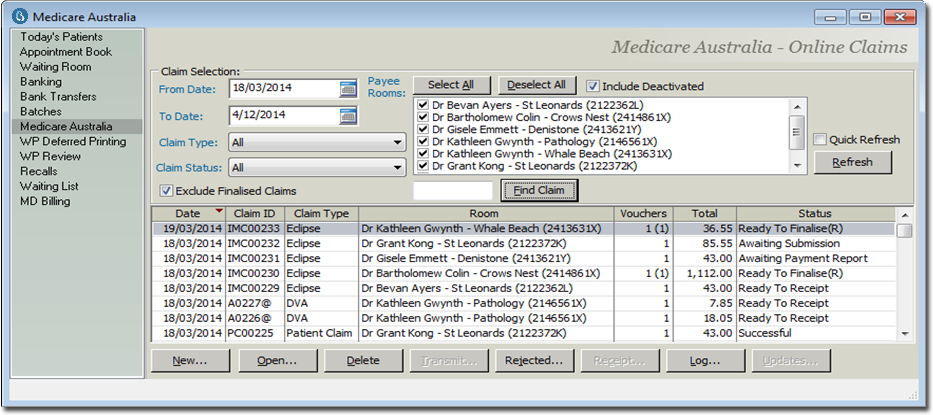
When Bulk Bill claims (without TYRO) are invoiced within the patient's account, the claim transfers to the Medicare Australia module. To access, open the Practice Explorer, and from the margin menu select Medicare Australia.
Due to the claims having not yet been submitted, they are not displayed on the main Medicare window. The New Batch selection holds the claims not yet batched, unprocessed, resubmitted either being looked into or ready to action (red in colour).
You can view claims associated with individual practitioner or all practitioners. You can examine claims within a specific , individual or all claim types, and indicate to display . When changes are made to these options, ensure you click the Refresh button or the check box is selected to auto-refresh the display. The status of claims determines the action required on the claim.
The following statuses will display once a Bulk Bill claim has been batched to Medicare:
| Claim Status | Description and Action |
|---|---|
| Awaiting Submission | Claim is waiting to be sent to Medicare. Click on the Transmit button. |
| Awaiting Processing Report | Waiting for the processing report for the claim. It can take up to 3 business days to process. Click on the Transmit button to retrieve the process report. |
| Awaiting Authorisation | Claim requires to be authorized. Open the claim and send to Medicare from the edit screen. |
| Awaiting Payment Report | Claim has been successfully processed, however awaiting payment report. It can take up to 6 business days to process. Click on the Transmit button to retrieve the payment report. |
| Ready to Receipt | Claim has been successful in processing and payment with Medicare. It is ready to receipt. Reconciling with the Bank Statement and payment is recognized, click on the Receipt button. Once receipted; the receipt will generate to the Banking, EFTPOS, as a Direct Debit payment. |
| Rejected | Items within the claim have been rejected. Click on the Reject button to display the Medicare Error Code & Description, and to decide to resubmit or write off the claim |
Procedure
-
From the button on the lower-right hand side of the screen, select from the margin menu.
- Select Practitioner, as and if required. If not selected from this window, these options can be selected when sending the Bulk Bill or DVA batch (next step).
-
To batch the new Bulk Bill claims, click New
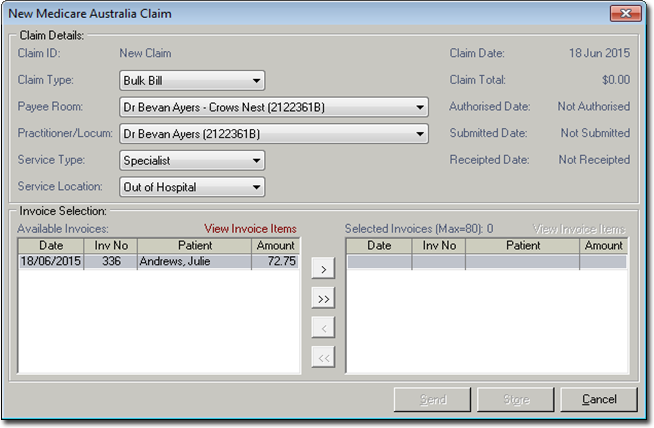
- The defaults to . Select the appropriate Practitioner and (if multiple are available), and if required.
-
Click
 to select a single claim, or
to select a single claim, or  to select all
claims. Ensure that the resubmitted claims (red in colour) are not included within
the selected invoices to batch, if you are only batching new claims.
to select all
claims. Ensure that the resubmitted claims (red in colour) are not included within
the selected invoices to batch, if you are only batching new claims.
- Click Send.
-
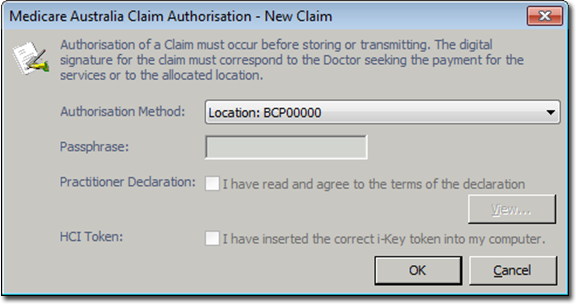
In the Claim Authorisation window, from the
Authorisation Method select a method if
required, or click OK.
-